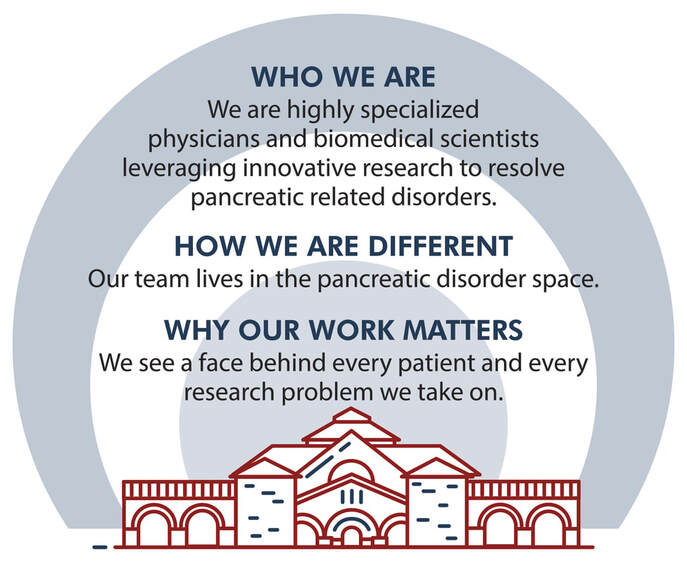
The Husain Lab at Stanford
Stanford University School of Medicine
Department of Pediatrics, Division of Gastroenterology, Hepatology, and Nutrition
1701 Page Mill Rd, Palo Alto, CA 94304,USA
Department of Pediatrics, Division of Gastroenterology, Hepatology, and Nutrition
1701 Page Mill Rd, Palo Alto, CA 94304,USA